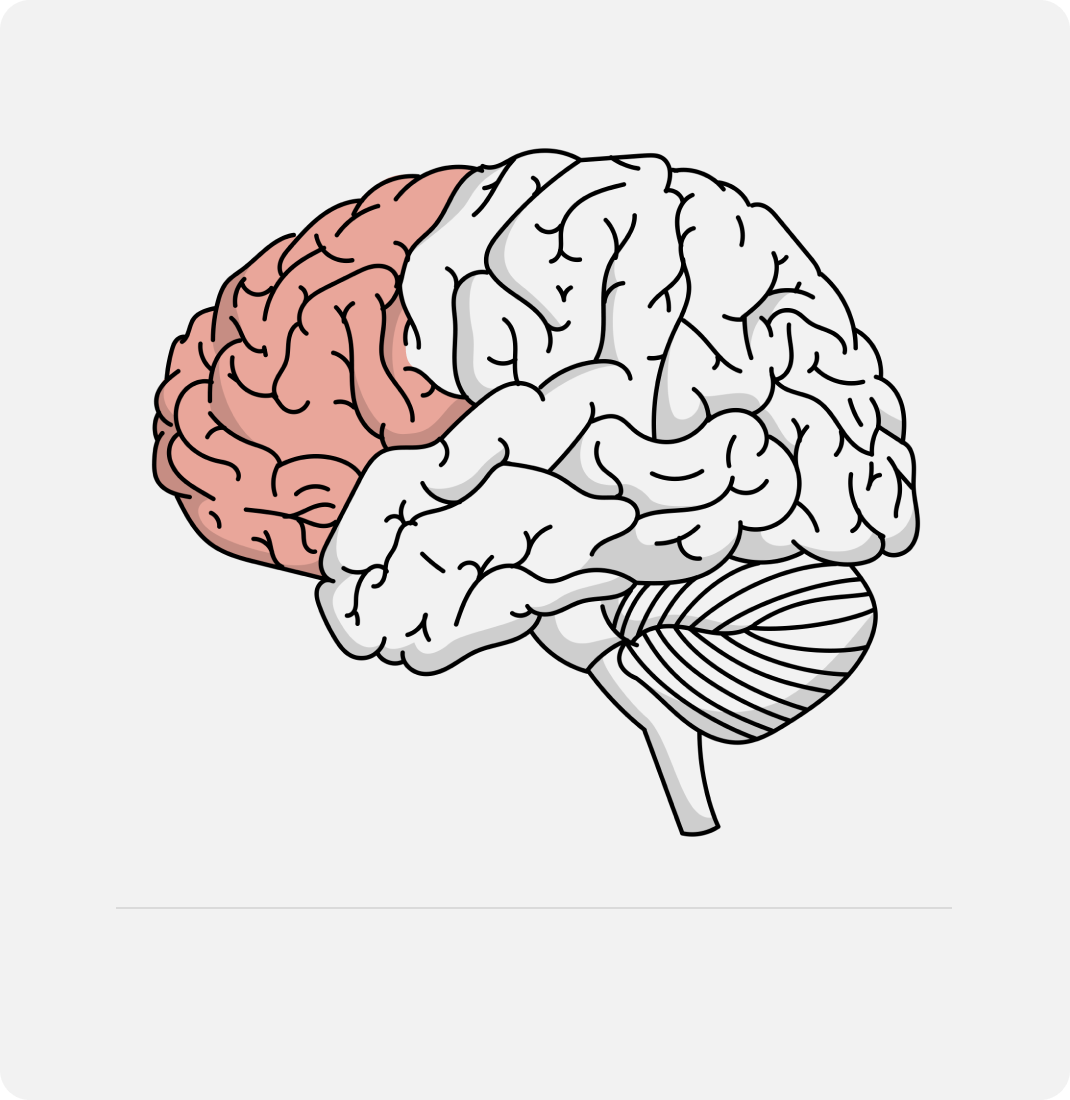
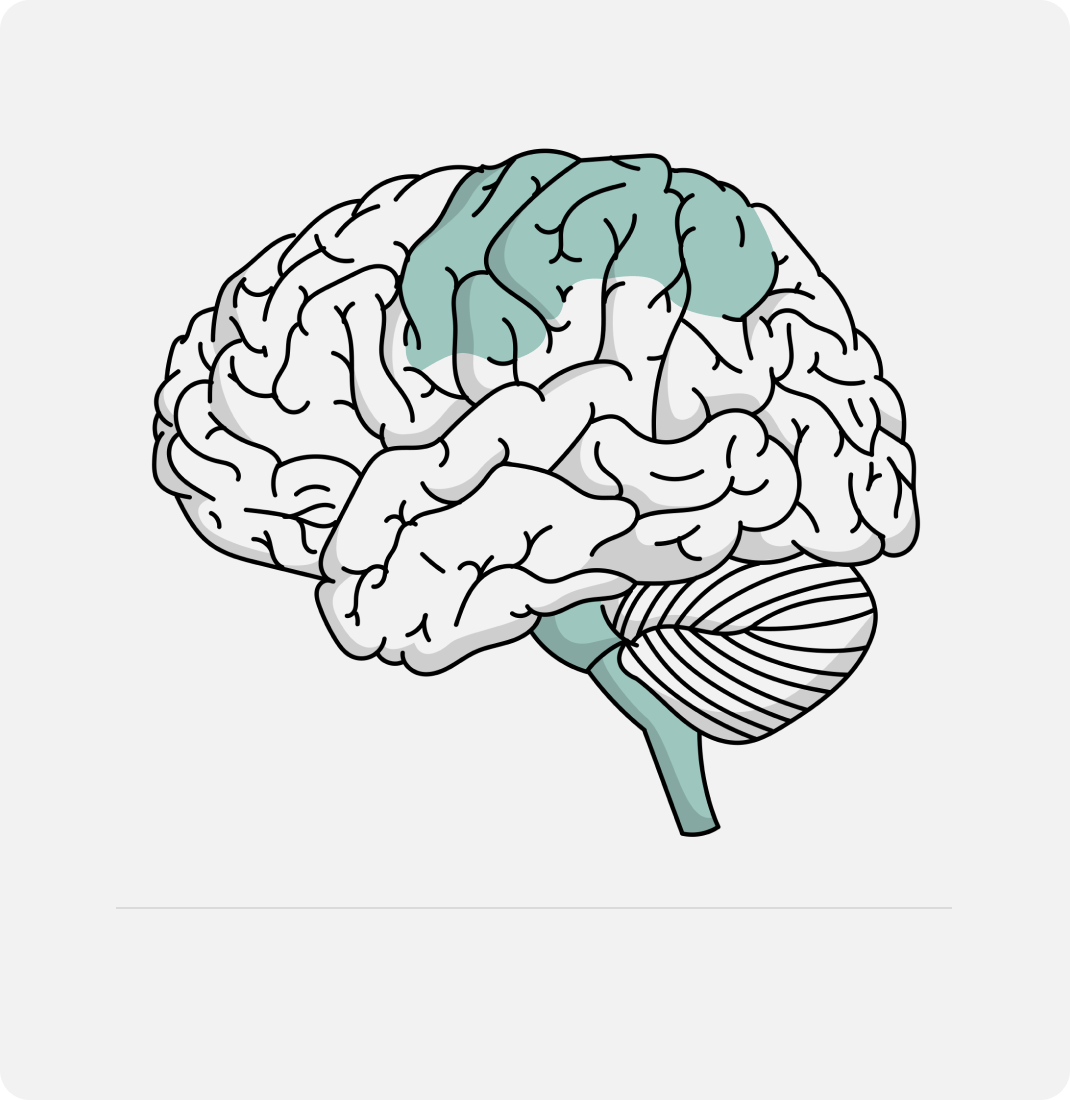
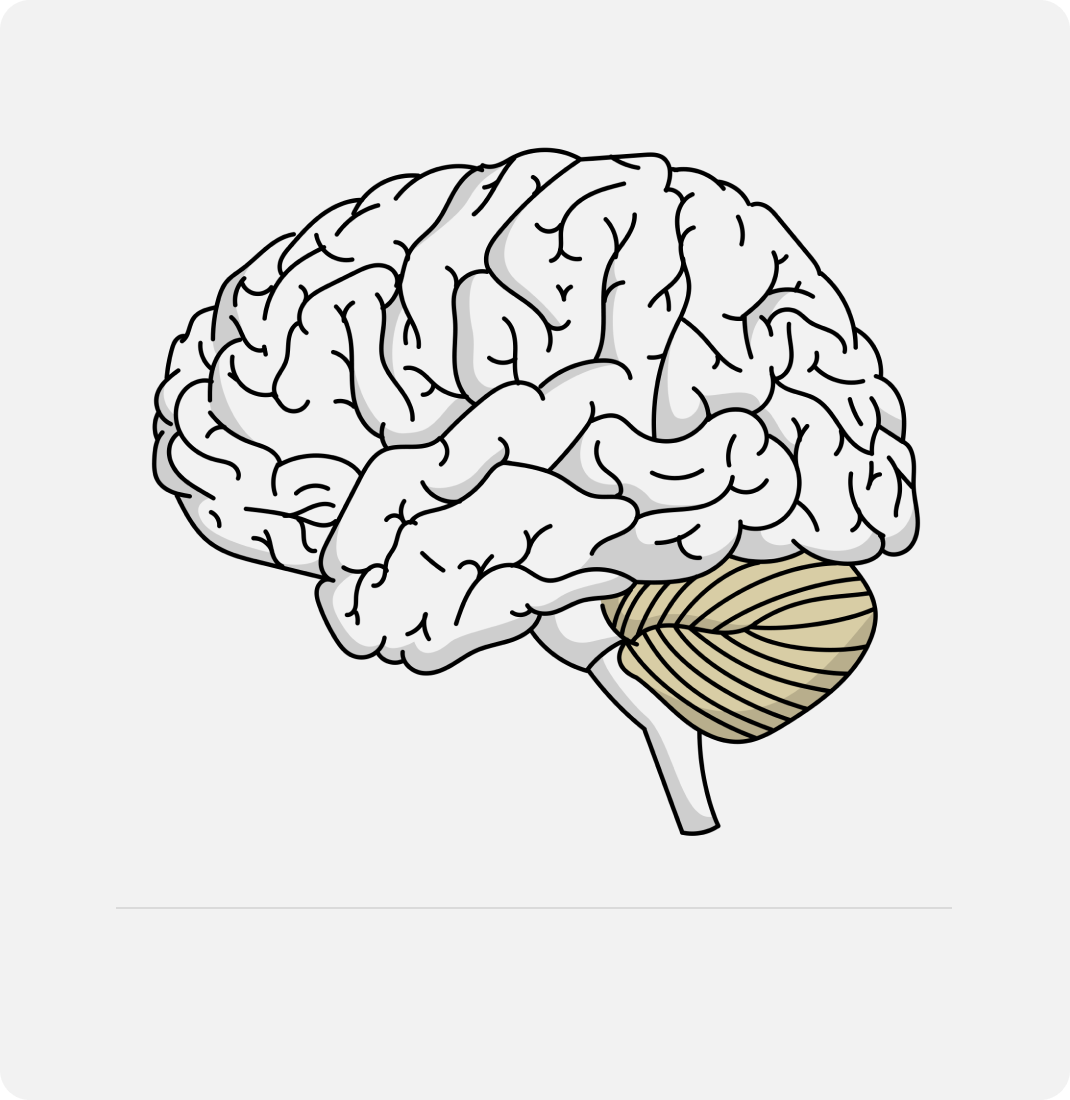
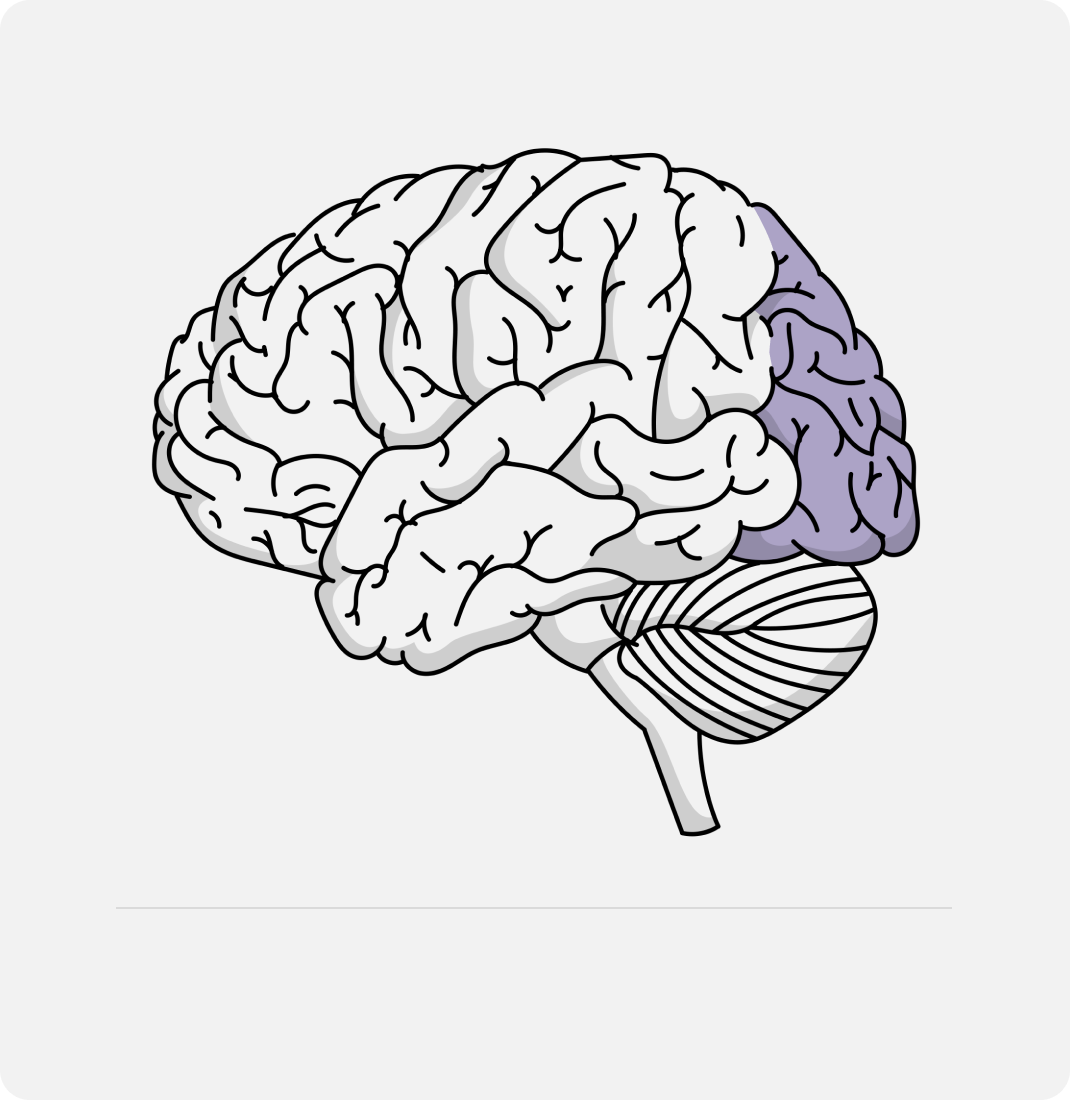
The functional impairment can be classified within nine neurodevelopmental domains.
The diagnosis of FASD requires severe impairment in at least three of these domains.
People with FASD have their own individual strengths and interests, but all experience a degree of difficulty in everyday activities and will likely need additional support to thrive.